There is a great deal of frustration about the uncertainty surrounding the Covid-19 pandemic. It seems that almost from the very beginning, what we didn't know about the novel coronavirus vastly outweighed what we did know, and as with so much else in life, that uncertainty was paralyzing at times.
Fast-forward 10 months, and we have learned a great deal. For example, we have a much better idea of the more worrisome risk factors for severe disease like obesity, age over 75, cardiovascular disease, and diabetes. Moreover, in an extraordinary feat of scientific ingenuity and dedication, we have several mRNA vaccines now being delivered to people around the world. In so many ways, it feels like we have finally started to get a handle on understanding what we are facing, and that has been no small source of comfort for many of us, ranging from physicians like me to every man, woman, and child across the nation who has worried about themselves and their loved ones.
Recently, however, a new source of uncertainty has arisen in the form of a variant in the novel coronavirus that has spread quickly. There are many concerns about what this means for the next stages of the pandemic, especially as we stand on the brink of the largest mass vaccination effort in recent memory — not least of which, will this new variant derail all of the hard-earned progress on the horizon that the vaccinations and social distancing efforts have bought us.
Fortunately, there are some key elements of information regarding the new variant that we already know. It was first identified in the United Kingdom in September 2020, according to the Centers for Disease Control, and has since spread to a number of countries across the world, including the United States as of December.
It isn't surprising that there is a variant of the novel coronavirus; viruses often go through a number of mutations that affect their ease of spread and virulence (how sick they will make someone), which is part of why the seasonal influenza virus changes from year to year. Moreover, the novel coronavirus that causes Covid-19 itself has had several variations that have been identified and tracked over the past year before the U.K. variant became notable.
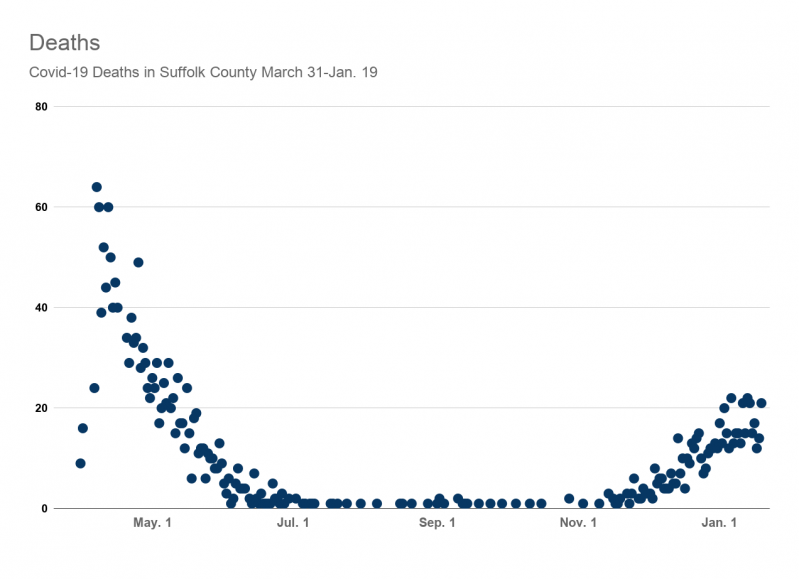
What seems to make this variant worth watching, however, is that it appears to have higher transmissibility than the previously dominant forms of Covid-19. In other words, it may be easier to catch and may spread faster. Obviously, this is of concern in areas like the United States, where regional health care systems in a number of areas are already strained to their limits. (We remain fortunate here on the East End of Long Island not to have reached that point yet.)
Importantly, the U.K. variant does not appear to have higher virulence, or a higher likelihood of causing more severe disease, according to the data gathered to date. This, at least, is reassuring, as are the announcements from Moderna (on Dec. 23) and Pfizer-Biontech (on Jan. 8) that early studies indicate their respective vaccines appear able to protect against the U.K. variant of the novel coronavirus.
Obviously, all of this is still very early in terms of information gathering. As throughout the rest of the pandemic, what public health officials and scientists know and say will change as new information becomes available. While this can be a source of anxiety and unrest, we have to remember that it reflects a dynamic situation, one that thousands upon thousands of health officials, scientists, health care workers, and governments are working tirelessly to grapple with. If the last year has taught us anything, it is that the progress we can make when these groups across the world come together can be astounding in terms of scientific developments, and I would expect to see that continue as we learn more information about these new variants in the novel coronavirus.
In the meantime, the best thing we can do is to keep doing what we have been doing — staying safe by wearing our masks and social distancing and seeking new information from trusted, reliable sources.
Joshua Potter, D.O., a physician with Stony Brook Southampton Hospital's Meeting House Lane Medical Practice, oversees the practice's Shelter Island office. He specializes in family and neuromusculoskeletal medicine. Opinions expressed in this column are his personal and professional views and not necessarily those of his employer.